The Double Life of Retsef Levi
What was an MIT mathematician doing at a vaccine injury roundtable in 2021? How, four years later, did he end up on the Advisory Committee on Immunization Practices (ACIP)? What about the comments he made and questions he asked at the last ACIP meeting - were they reasonable?
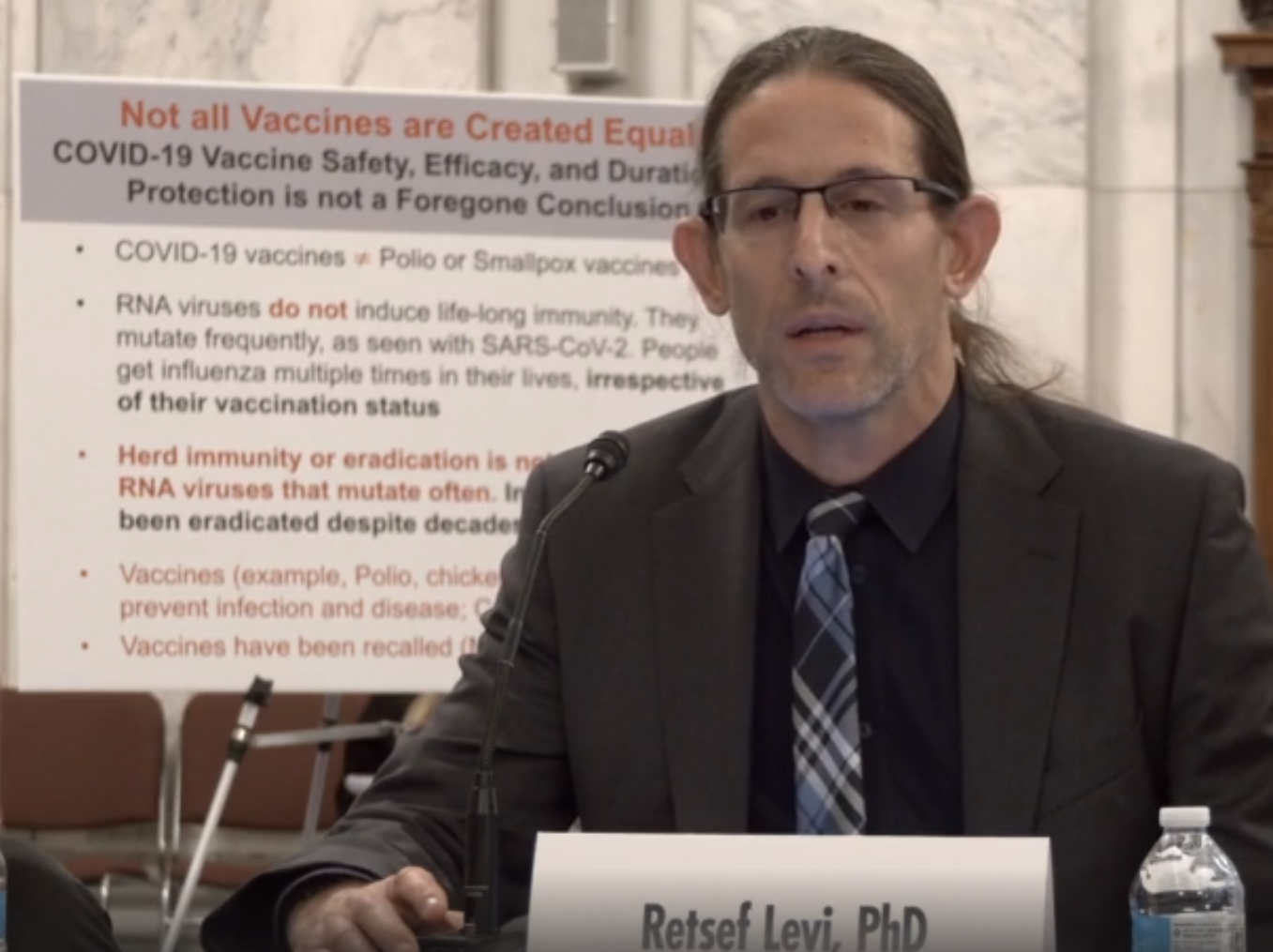
An “Independent thinker” joins the Advisory Committee on Immunization Practices
By Alex Morozov
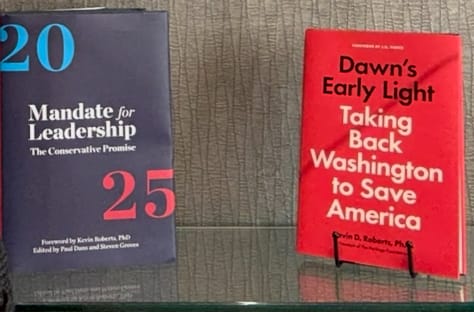
Dr Retsef Levi and Aaron Siri presenting at Sen. Ron Johnson’s Expert Panel on Federal Vaccine Mandates and Vaccine Injuries, US Senate, November 2, 2021.
July 10, 2025
According to my unofficial count, Senator Ron Johnson of Wisconsin holds a modern Senate record: five “roundtable discussions” in the last five years (the closest second is two). They are held in the historic Kennedy Caucus Room, are open to the public and are broadcast live. Given his controversial views - he suggested mouthwash as an effective COVID-19 intervention, among other misinformation - these events showcase the “who is who” of the anti-establishment world.
At the November 2, 2021 event, several patients gave tearful testimony, describing complications they suffered after receiving COVID-19 vaccines. Aaron Siri gave a presentation, mentioning his antivax law firm with a staff of 20 (it’s now up to 40). He was at the time the lawyer for the Informed Consent Action Network, an anti-vax nonprofit started by Del Bigtree when he and Andrew Wakefield made their first documentary, Vaxxed, in 2016.
One person, however, was an unlikely presence: Dr Restef Levi, a Professor of Operations Research at MIT. His two most recent research papers are called "Competitive Algorithms for the Online Minimum Peak Appointment Scheduling” and “"Improving Farmers’ Income on Online Agri-Platforms: Evidence from the Field" (note the pun in the second one!)
What was a mathematician and Professor of Operations Research doing at a vaccine injury roundtable? How, four years later, did he end up on the Advisory Committee on Immunization Practices (ACIP)? What about the comments he made and questions he asked at the last ACIP meeting - were they reasonable? And why did he vote against recommending an RSV antibody, clesrovimab (Enflonzia, Merck)? This antibody, not a vaccine, is given once to an infant and lasts for several months, covering the entire RSV season. It reduces the rate of infant hospitalization due to RSV by 84% and was approved by the FDA just prior to the ACIP meeting.
This is a story about conspiracy beliefs. Half of Americans have such beliefs, perhaps you and me included. But equally, this is a story with implications of our the new US healthcare leadership for the future of ACIP, the future of clinical research, and the practice of medicine.
Levi declined to be interviewed for this story, citing “limited ability to interact with media.” He did, however, give several recent interviews to conservative outlets - “conspiracy-fuelled” Epoch Times TV and to Brownstone Institute’s Maryanne Demasi (twice). (Brownstone Institute, incidentally, was started and is led by Jeffrey Tucker, the mastermind behind the Great Barrington Declaration and such an extreme libertarian that he encouraged his teenage kids to smoke. My interview with him - in a future story.)
Levi’s recent interviews, and older archival material, paint a picture of his double life: one as an MIT professor, and one not obvious at all from his MIT website: a critic of the COVID response and a conservative darling. There was the Senator Johnson hearing in 2021; participation in the March, 2022 gathering of the Academy of Science and Freedom, the anti-lockdown group founded by Scott Atlas, Martin Kuldorff and Jay Bhattacharya, at the ultra-conservative Hillsdale College in Washington, DC. This gathering is where Levi met Tracy Beth Høeg. She is now a top adviser to Marty Makary (and previously a co-author of a misleading post with him). She is also “good friends” with Jeffrey Tucker and Joseph Ladapo, Florida’s surgeon general appointed by DeSantis. In 2023, Høeg hosted Levi as a guest on the podcast she runs along with Christine Benn, a vaccine expert often quoted by Kennedy. Levi himself said this about Ladapo: “A+ on intellect and moral compass to do the right thing! What public health needs.”
And since mid-2024, Levi (under a misspelled name) has been on the editorial board of Science, Public Health Policy and The Law, the antivax (according to another editorial board member) journal that published, with Andrew Wakefield’s help, the famous Mawson paper that helped Kennedy pass his confirmation hearings. But Levi doesn’t list this editorial position along with a few others on his MIT CV.
Searching for the moment when the second life appeared, I pieced together his bio.
Levi was born in an industrial Israeli town of Kfar Saba, one of eight siblings. His father was a journalist and a veteran of the Stern Gang, an extremist zionist organization. “Levi seems to have inherited [his] parents’ penchant for challenging their surroundings,” reflected an Israeli journalist, Haaretz’s Meirav Arlosoroff.
Levi served in the Israel Defense Forces as an intelligence officer - “special forces,” as he described it - for 12 years, well more than the mandatory 2.5 years for Israeli men. His subsequent career path seemingly had nothing to do with healthcare: math at Tel Aviv University, PhD in operations research from Cornell. His PhD thesis is called “Approximation Algorithms for Stochastic Inventory Control Models” - nothing health-related.
However, once he joined MIT in 2006, he started a collaboration with Mass General Hospital to improve the scheduling of surgical patients, which ultimately grew out into a new department at MGH, Healthcare Systems Engineering, that still exists today. By 2016, he was leading MIT’s Sloan School of Management’s Initiative for Health Systems Innovation (HSI). And a slight note of discontent appears: concerns with the status quo:
“...the current health system is designed to provide discrete, reactive care for sick patients, in specified locations, … the idea of health is going to be broader, more comprehensive—what do patients eat, do they smoke, where do they live? It’s going to require us to think deeply about what we do for every patient, and how we think about the welfare of the population.”
When COVID started, Levi immersed himself in pandemic response. He joined MIT’s “COVID-19 Policy Alliance,” was interviewed by the Washington Post about the risk of “hospital collapse,” and helped multiple other researchers as evidenced but acknowledgements in many research papers.
He also embarked on his first COVID-related research project together with a trainee, Christopher Sun, a Canadian postdoctoral fellow with a dual appointment at Levi’s MIT Sloan School of Management and the MGH Healthcare Systems Engineering department and with significant prior healthcare operations experience.
Levi’s frustration with the US response was becoming apparent - “We definitely did not perform very well as a country compared to other countries,” he said in May 2020.
But one “other country” did not do well, either, in Levi’s mind: Israel. In mid-2020, at the invitation of Israel’s Education Minister, Yoav Gallant, Levi spent 6 weeks on a team of experts planning for safe reopening of Israeli schools. Arlosoroff described Levi as “mad over what he sees as the unnecessary closure of the education system.” The government decision-making process was “unprofessional, not transparent, based on the belief that the only effective response to the pandemic is a strict lockdown, with no effort made to pinpoint high-infection areas and crack down only in those places,” she quoted Levi as saying.
He made some proposals on optimizing healthcare response, as well: reducing personal protective equipment for healthcare workers, bringing in retired doctors, and shortening the quarantine period. “Levi’s proposals aren’t necessarily right, but he isn’t alone in his criticism,” commented Arlosoroff. “Their criticism resonates because their claims aren’t considered at length, and because it’s clear that what is being done has failed,” she astutely observes.
Mid-2020 is when Levi and Sun embarked on their second COVID-related project that appears to be the pivotal point in Levi’s career bifurcation, and likely earned him the invitation to Ron Johnson’s 2021 gathering.
It all started with the news of myocarditis as a complication of COVID-19 and, to a lesser extent, of the vaccines. Levi recalls reading about myocarditis and how much of it can go undiagnosed. If there was an increase of undiagnosed myocarditis in Israel after the COVID vaccine rollout, how would we know? He then came up with a brilliant way: by analyzing ambulance calls during the 3rd COVID wave in Israel when vaccines were rolled out, and comparing that to the prior wave when vaccines were not yet available. Any difference would be solely due to the vaccine, Levi apparently reasoned. (Or so he thought - variants were not commonly discussed back then).
The paper, which ultimately was published in April 2022, is remarkable in that it is all about one curve: the number of ambulance calls (in Israel you dial 101, not 911) per week, over about a 2-year period. You can see this red line zig-zagging up and down across the page, like a mountain range. On a slow week, there were 4 calls (only calls for heart-related issues, and only in young people, are plotted, so the numbers are very small). On a busy week, 9 or 10 calls. There was one week that had 11 calls (on the right side, second peak from the right), that happened to coincide with the main COVID-19 vaccine rollout in Israel.
I will ask a question here - look at this red peak, that extends just slightly above the 10 line. Does it look that different to you from all other peaks? To me it does not. So whatever happened at the same time - maybe it’s an earthquake, maybe it’s some stars aligning, maybe it’s someone’s prayers - we really cannot conclude that this little peak was caused by this. It’s just ups and downs of a random curve - noise. If nothing else, note how the difference from week to week is just a few calls. If one or two extra calls happened on a different week, then that week would be the top peak.
You see how seeing more than just noise here could be described as “illusory perceptions of pattern and causality?” More on this later.
But Sun and Levi came to a different conclusion. Doing fancy math, they try to show that this peak’s timing was not a coincidence. Plus, as Sun and Levi acknowledge, they didn’t know who these patients were, whether they were actually vaccinated, and what was their final diagnosis.
Surprisingly, they don’t even describe what we call the “demographics” of the patients - their average age, % males vs females. That is usually “Table 1.” Any clinical researcher will know this concept of “Table 1.” Whenever you are describing a group of people - clinical trial, observational study, etc - you always start with Table 1 that tells us about this group. In this case, we know that our starting point is the “under 40 population in Israel” as the title of the paper says. Or is it our starting point? What was the total under 40 population of Israel when the study was done? How many were there? What was their average age? Is it 20? 15? 25? What is their men-to-women ratio? The paper doesn’t say. And by the way, did it remain the same over the course of the study, from 2019 to 2020 to 2021? Not clear.
OK, so maybe that is not our study population. Then what is? There is a section in the paper called “Data sources and study population.” But this section doesn’t say anything about the study population. It describes two “datasets” - one is the dataset of emergency calls - “all the calls received through Israel’s national emergency telephone number (1-0-1)”. The other dataset is vaccination and COVID-19 cases. “Data on the vaccinations and COVID-19 cases were obtained from the online Israel Government Database Portal.” OK. So what is the study population? Is it the calls combined with the vaccination and COVID cases? We cannot do that because they are not linked. We don’t know who called. So there is no study population in this study. That’s why there is no Table 1.
Why is this important? Well, first because it’s in the title of the paper. But also, critically - OK, so we had 8 calls one week, 10 calls another week, etc, out of how many people? How many people age 16-40 are actually in Israel, and what are their typical ailments, typical reasons for why they call? So we can say, “usually, when someone age 16-40 has chest pain, it’s usually myocarditis. Or it’s usually they pulled a muscle playing soccer. I don’t know. And to answer that question, we need to know more about this population.
There was one study in 15-33-year olds seeking emergency care for chest pain in the UK. More than half turned out to have non-cardiac origin, such as musculoskeletal, gastrointestinal or respiratory. Does this paper apply to Levi’s study? I don’t know. He says it’s 16-40, so it’s kind of similar. But is it mostly 16-year-olds, with a few 40 year-olds, or vice versa? Does Israel have more men than women, or vice versa? Where do they live? Maybe the emergency calls came from the North of Israel, and COVID cases were more in the South? I don’t know… With this basic problem - no Table 1 - I can confidently say, and I hope you will agree, this is not a quality study.
But there is more - some math “sleight of hand” that is evident. If you look carefully, the points on the graph do not correspond to whole numbers - like the lowest point is almost at 4 but not quite. If this is the number of calls per week in all of Israel, how can this be that there was 4.2 calls that week?
Well, it turns out, these are not actual numbers of calls each week, but a 5-week “moving average” - taking a window of 2.5 weeks before and 2.5 weeks after, and calculating an average for the 5 weeks, and then putting that number on the graph. Why did they do that, and why did they pick 5 weeks? They don’t explain. Similarly, they present a “sea of numbers” - comparing 2019 to 2020 to 2021 to whole year, vs just January to May, total, under 40, over 40, males under 40, females over 40, etc, etc. They calculate a % increase and a p value for each one, and then pick out those that look high - like females under 40, specifically for “acute coronary syndrome.” There you see about a 35% increase from the pre-vaccination period. But if you look at males under 40, for “cardiac arrest” specifically, there is no statistically significant increase.
This kind of a “fishing expedition” is a statistical no-no. The more you “slice and dice” the data, the more things you find. But most will be due to chance: if you repeat the study, the pattern may be totally different.
A leading statistician, Thomas Fleming, whose name is instantly recognized by clinical researchers as the developer of “The O'Brien-Fleming boundary,” explained this well in an article called “Clinical trials: discerning hype from substance.”
He once visited a hospital nursery, and noticed that there were 20 newborn boys and only 2 newborn girls. Being a statistician, he calculated a p value to see how likely this could have occurred by chance, given that generally numbers of boys and girls are approximately equal. The p value was 0.0001. In other words, if one were to visit 10,000 nurseries, only once would one expect to observe such an imbalance. Yet, it’s clear that Fleming had not visited so many nurseries - this could have been his first visit, in fact. The explanation for this paradox is that he did not go into the nursery with the plan to study the ratio of boys to girls. This was just one of many observations he made. Maybe he could have seen several cars of the same make in a row, or several people with the same name, etc.
“The interest in being able to interpret and report results in clinical trials as being favorable is pervasive throughout health care research,” he cautions. “In exploratory analyses, P values will be misleading when the actual sampling context is not presented to allow for proper interpretation, and the effect sizes of outcomes having particularly favorable estimates are probably overestimated because of "random high" bias.”
Then there is another problem. Look at the little peak again where the line goes above 11. This means that there were two extra calls that week. Two calls. Two people, somewhere in Israel, picking up the phone and calling 911. We don’t know if those two people were vaccinated or not, we don’t know what the doctors found at the end. Maybe it was nothing. So this entire paper is based on ups and downs of very, very small numbers - one or two calls here and there across all of Israel, a country of 6 million people.
So many limitations of Levi’s study, yet only one - lack of follow-up - is acknowledged by the authors. Even when faced with implausible observations - why the see more cardiac events in females, while COVID myocarditis is more common in males, the authors attempt to rationalize them, rather than admitting that it’s likely a chance finding: “This may suggest the potential underdiagnosis or under-self-reporting of myocarditis in females.”
At the end, Sun and Levi conclude, “While not establishing causal relationships, the findings raise concerns regarding vaccine‑induced undetected severe cardiovascular side‑effects and underscore the already established causal relationship between vaccines and myocarditis, a frequent cause of unexpected cardiac arrest in young individuals.”
Do they? Given the massive limitations of the study, to me it does not “raise concerns.” What is the basis for mentioning “severe cardiovascular side effects?” We don’t know the diagnosis these patients received, and what proportion was cardiovascular. We don’t even know whether these patients received the vaccine. And how did myocarditis get into the concluding sentence? If I described this as ““connecting the dots” that are not connected, would you agree? More on this later.
If I were in the Israeli Ministry of Health, or at the FDA, and I got this paper, I would not find it “actionable,” i.e. I would not be sure what to do about it.
But that is not how Levi saw the findings. At the Ron Johnson Rountable, he is visibly tense, his neck veins puffed up. “I am not an antivaxer. I am not a republican, I am not a democrat. I am just a scientist who challenged the current narrative that dominates public health policies around the world, in the US and in Israel.” “I know many scientists who like me think that the current narrative is very extreme and wrong. But very few of them are willing to speak up. And I am not sure I can blame them. Any attempt to deviate from the main narrative today is faced with a wall of hostility, rejection, and even elimination.” He quoted a senior colleague at MIT who warned Levi, “you have to be careful, or you can be eliminated.”
“Me and my co-authors pointed out that if you look at national emergency service calls in Israel, you see a dramatic 25% increase in these calls… in parallel to the vaccination campaign,” he announced to the stunned room. “We wrote a paper about that, not claiming that we have a causal effect, because we don’t have a proof for that, but we did raise the concern, and we called the authorities to check what is going on. Needless to say, we never got a response from the authorities.”
First, this is not entirely consistent with his other descriptions of the “saga.” In another video he did say the FDA called him back right away. It was the Israeli Ministry of Health that never responded.
But second, why “needless to say?” Is it a foregone conclusion that “the authorities” do not care about safety? Or maybe there is another explanation - they just didn’t consider this study to be reliable or “actionable?”
Levi continues, in a way supporting this last explanation. “In fact, they went public and called this research ‘fake’. But even more concerning - journal after journal after journal in the academic literature is rejecting this article, most of the time based on the argument that…” He leans into the microphone and looks at Senator Johnson, “‘...it is not a priority!’ Well, I don’t think calling safety concerns ‘fake’ is morally right, or scientifically right.” (3 weeks after this event, Sun and Levi submitted the paper to Nature’s Scientific Reports, the world’s 6th most-cited journal, and it was published a few months later).
Here, for me, the logical leap is on display. My paper was rejected by multiple journals, my concerns were not taken seriously by multiple regulatory agencies - that’s not because there was anything wrong with my paper, but because there is a coordinated effort between the journals and agencies around the world to cover up the truth, this logic goes.
“Once healthcare agencies decided to give this vaccine to all ages, including young people that are not high risk, they committed themselves to a path that they cannot admit to any wrong,” Levi said in Høeg’s podcast in 2023. That’s the reason why we see denial and efforts to suppress any efforts to understand what the risks are, in spite of mounting signals.”
Just for the record, I’m not aware of any evidence that global health authorities were purposefully hiding safety signals for COVID-19 vaccines, or any other product, for that matter. Janssen’s vaccine was restricted by the FDA after a safety signal emerged, for example. And a few months before Levi’s presentation at the roundtable, EU regulators announced a “possible link” to “very rare cases of unusual blood clots” with the Astra Zeneca vaccine.
But on Høeg’s podcast, this perspective was lacking. “I think that’s so important, and podcasts like this are important too, to talk about our experience as researchers,” Høeg concurred with Levi, while Benn nodded. “And this is where I bring my intelligence hat,” continued Levi. “Before coming to academia, I spent 12 years in intelligence. Often we say, ‘oh, this indication doesn’t prove it,’ ‘this finding doesn’t prove it.’ But you have to step back at some point and look at the mounting evidence and say, ‘Hey, something is wrong here.’”
Why would a researcher compare his struggles to publish a paper to the work of a military intelligence officer piecing together clues about the enemy? “Well, it’s important to know, we are not conspiracy theorists,” jumped in Høeg to clarify.
What could she be referring to?
Karen Douglas at the University of Kent in the UK is one of the world’s leading experts in conspiracy theories. “The most common feature of a conspiracy theory is that something is being covered up,” she explained in a recent interview. “I have always been interested in the psychology of attitudes and attitude change. I have also studied how people’s behaviour is influenced by new communication technologies. A few years ago, I came across some conspiracy theories online while looking for study materials on another topic, and I became intrigued by them.”
So many of us believe at least one. This table in a recent paper (ironically in the same journal as Levi’s) is striking:
How does this happen? In 2022, Douglas published a paper called “Rabbit Hole Syndrome: Inadvertent, accelerating, and entrenched commitment to conspiracy beliefs.”
She describes “ central features of the rabbit hole concept in lay usage. You can be drawn into it incidentally and find it difficult to get out of. It then draws you ever deeper, in a non-linear descent… Thus, like the term ‘conspiracy theory’ itself, the rabbit hole metaphor is not necessarily pejorative”
“People do not enter the process intending or even expecting to develop a deep commitment to conspiracy theories. Their attention, like Alice’s, may be captured by something interesting or appealing… Importantly, people appear unable to detect how exposure to conspiracy theories changes their beliefs and so may not notice what is happening to them in these early stages of Rabbit Hole Syndrome.”
Then comes acceleration, due to a “vicious cycle” - “As conspiracy beliefs increase, people increasingly identify with other believers, adopting identities, such as “truther” or “critical free thinker” that, in turn, encourage deeper commitment to these beliefs… illusory perceptions of pattern and causality (e.g., in coincidences and in art) seem to play a role in conspiracy belief. As conspiracy theories become more salient in people’s representations of the world, they can become the very stimuli between which people “connect the dots.”
Smart or even academically brilliant people are not immune, writes David Robson, the author of “The Intelligence Trap: Why Smart People Make Dumb Mistakes.” In one study he describes, “more educated participants seemed less likely to update their beliefs after they had been debunked; instead, they actually became more certain they were right. Somehow, their greater knowledge simply allowed them to dismiss the new information and harden their attitudes.”
In March of this year, Levi posted on X: (my correction in red)
(He then describes some concerns with another trial, HARMONIE)
There are three mysteries about this post. First, what prompted it? He referenced two New England Journal of Medicine articles, one from 2022 and one from 2023. Nirsevimab was approved in the US and Israel in 2023. There was no nirsevimab news. Levi would not be appointed to Advisory Committee on Immunization Practices (ACIP) until June 9, and the agenda (that included nirsevimab) would not be published until June 18.
The second mystery is Dr Efrat Schurr, whom Levi thanks for “collaborating on the analysis” at the end of his post. She is also Levi’s only co-author on two papers - one on COVID-19 vaccine safety during pregnancy, and one on risk of miscarriage after COVID-19 vaccination. Schurr is not an obstetrician, however - she is a pediatrician, currently practicing in Jerusalem, Israel with no apparent academic affiliation. And it’s not clear that she has expertise in the research methodology on which her papers with Levi are based, judging by her three publications in addition to the two with Levi. As a matter of principle, I would expert an obstetrician, someone who takes care of pregnant women, to be an author on a paper discussing pregnancy. And why would a full professor at MIT co-author a paper with a pediatrician with no academic affiliation, about obstetrics, a different area of medicine? It’s a mystery I have not yet solved.
The third mystery is whether Levi tried to find answers to the concerns he raised, perhaps by talking to experts, before or after posting them on x. Does not appear that this happened, and even the mistake of mixing up the studies remains uncorrected.
A few months ago, The Lancet, a top medical journal, had a special issue devoted to RSV. In an accompanying video, Dr Ruth Karron of Johns Hopkins University presents a striking number: 33 million children getting sick and 100,000 children dying each year due to RSV around the globe - the second most common cause of death in infants after malaria. Most of the deaths are in previously healthy kids.
There is still no treatment.
Remarkable progress was achieved in 2023, Dr Karron says, with the introduction of a vaccine and a long-acting antibody. But they are only available in high- and middle-income countries, not in low-income, such as Kenya. Why is this a problem? Two reasons.
One, low-income countries have very few intensive care facilities, leading to high mortality, says Dr Natalie Mazur, a Dutch pediatrician. A “bandaid” solution was proposed - high-flow nasal cannula - basically forcing a lot of oxygen through a small tube - but Dr Mazur’s study showed that it’s ineffective or even harmful. “Prevention is key. We are in an exciting new chapter now that RSV can be considered a vaccine-preventable disease,” she says.
The second problem is long-term complications. Dr Heather Zar, a Professor of pediatrics at the University of Cape Town in South Africa, says that RSV infection in early life can lead to stiffer lungs, which can impact life expectancy.
“The full public health value of these new RSV prevention products is likely greater than what is measured by early life RSV disease.”
I’m not sure whether Levi is familiar with any of this, or talked to any of these researchers.
But it appears that at the ACIP meeting on June 25-26, 3.5 months later, his concerns remained unresolved. Recall that in early June Kennedy fired the entire ACIP and appointed several new members, including Levi.
At the ACIP meeting, nisrevimab was actually not on the agenda, but rather a newer, similar antibody called clesrovimab that binds to a different part of RSV. It was just approved for healthy infants by the FDA a couple of weeks earlier, and the question was whether ACIP agrees (FDA approval happens just once, whereas ACIP may review these products - vaccines and rarely non-vaccines such as antibodies - on an regular basis, as rates of infection change, epidemics emerge, etc). Dr Adam MacNeil, PhD, MPH, Deputy Branch Chief for Epidemiology, Respiratory Viruses Branch at the CDC, went over a presentation of the risk-benefit analysis that he said was prepared by a working group including “CDC and external experts.”
In the US, to this day, tens of thousands of children are hospitalized (80% of these are healthy before RSV; and have the risk for long-term lung stiffness and other complications from RSV), and a few hundred die from RSV acutely, MacNeil said - not counting those whose life is cut short due to lung stiffness in their adulthood.
After reviewing the benefits and harms in detail, Dr MacNeil presented the working group’s recommendation: Approve.
Levi was first to ask a question. “I would like to share data that I found and would be happy to hear the reactions of the colleagues at the CDC,” he said. He then proceeded to repeat his concern #1 from his March 4th post - in the nirsevimab trial called MELODY, there are more deaths among children receiving nirsevimab compared to placebo. Isn’t that concerning?
It turns out, a quick look at the FDA review would have addressed that concern. FDA review documents for every drug are posted on a portal called Drugs@FDA. I immediately went there to look.
Under “Key safety issues,” there is a section called “Imbalance in Deaths During Clinical Trials.” It says, “There was an unexpected imbalance in the number of deaths observed in subjects who received nirsevimab compared to in subjects who received controls (placebo or palivizumab). Therefore, deaths in all trials were carefully reviewed to determine if any death might be related to nirsevimab.”
There is a nice summary of all the trials:
And yes, there is an imbalance - 12 deaths out of about 4000 children, versus 4 out of about 2000 (there are only half of patients on the placebo across the trials because the trials used what’s called 2:1 randomization, so each child has double the chance to get the drug). So basically if we imagined there were 4000 on placebo, we would expect 8 deaths. 12 vs 8 - an imbalance. And I am not a statistician, but I asked ChatGPT, “What is the p value for 12 out of 4000 vs 4 out of 2000?” It produced a page worth of formulas, and then gave the answer - 0.4. Basically, this is totally random. So if you go to one casino, and you hit the jackpot 12 out of 4000 times, and in another casino 4 out of 2000 times - don’t pick the first casino. You have no idea which one is better. Total random chance.
But to be sure, the FDA reviewed each of the 12+4=16 deaths. There is a 2-page table that outlines them. (The trial was done in multiple countries, so only one of the 16 deaths occurred in the US.) One child in Panama was hit by a car. A child in Bulgaria was born infected with another virus, CMV. A child in Mexico had severe heart defects. The child in the US was born with a brain tumor.
Reviewing these deaths, the FDA concluded, correctly in my opinion, that the imbalance of effectively 12 vs 8 deaths, given so many of them are clearly not due to drug, was due to random chance.
Now, this document dates from May 2022, and is easily available online. Why didn’t Levi review it? It took me just a few minutes. Plus, he could have asked the FDA - he is a government official now. Instead, he repeated verbatim the same question he posted on x 3.5 months ago.
Then, his concern #2 - no surprise - also essentially exactly his concern #2 from his x post. Even though the numbers in the post were from another trial, the basic question remained the same: “Why do you see the same rate of infections (including RSV) in treatment vs. placebo arms (4.6% vs 4.9%), if this drug is supposedly reducing RSV infections by 75%?”
Yes - why is that, I thought. Shouldn’t we expect the rates of infections to drop?
This answer was also easy to find - just a quick look at the HARMONIE protocol (part of the trial publication).
It turns out that a bunch of smart people who designed this study 6 years ago - in early 2019 - thought about this issue very carefully. Here is what they came up with:
In this study, LRTI [lower respiratory tract infections] hospitalizations of any cause including RSV LRTI hospitalizations, occurring up to 6 months post-dosing/randomization, constitute the studied clinical outcome of interest; that is, they are constitutive of the efficacy endpoints. As a consequence, LRTI hospitalizations of any cause, including RSV LRTI hospitalizations, occurring up to 6 months post-dosing/randomization, will not be considered and reported as SAEs.
So the answer to Levi’s question is very simple: the RSV hospitalizations don’t show up in the safety section, that’s why you don’t see the difference.
In contrast, Levi, not knowing this simple explanation, constructed a more complicated and scary explanation - that while the RSV infections are reduced by the drug, some other mysterious side effects are taking their place. And he was holding his concern to himself for 3.5 months, just to raise it at the meeting. In fact Dr MacNeil’s presentation was on day 1 of the ACIP meeting, it ran late so they postponed the Q and A until day 2 - so Levi had to hold his question for one extra night to “drop the bomb” the next morning.
He then turns to clesrovimab which is the actual topic of discussion. “If I look on the clinical trials of the product we are supposed to vote on today, clesrovimab, again, a trial of 2:1 [randomization], there is again imlabance of 7 deaths to 3.
Let’s pause here for a minute. Here is a full professor at MIT. The trial is 2:1, meaning there are twice as many kids getting clesvorimab as placebo. How can he conclude there is an imbalance? What did he expect, 3.5 deaths on the placebo arm? I could not believe what I heard, and I thought you might not believe me, so I added a screenshot below.
But then he does drop an actual bomb. “And it seems that there is an ongoing trial with clesrovimab in infants with comorbidities, 1:1 randomization, it does report 8 to 4 deaths. I would like to hear from our colleagues at the CDC - should we be concerned?”
This question was passed on to Merck who said that similarly to nirsevimab, all deaths were reviewed and deemed not associated with RSV or interventions.
I went to Drugs@FDA to find the clesrovimab review document, but it was not there. So we do not have access to the table of deaths like we do for Nirsevimab. But a few questions this raises.
First, how did Levi find out about the 8 vs 4 deaths? This is actually very easy - it was part of Merck’s presentation at IDweek in October 2024, and was presented at the last ACIP meeting in November - both are available online.
Second, does this change anything? Also an easy answer: instead of waiting to drop the bomb at the ACIP meeting, why not talk to the FDA who approved this drug 2 weeks prior? Surely they reviewed and deliberated this in detail.
Third, what is the p value? There were 900 patients in the trial, 1:1, so I asked ChatGPT, “what is the p value for 8 out of 450 vs 4 out of 450?” The answer is 0.24 - also due to random chance (p value needs to be less than 0.05)
What if we were to combine both drugs? First, nirsevimab and clesrovimab are different drugs - they bind to different parts of the virus. So we should not consider them together. But even if we did for a second:
12/4000 vs 8/4000 (4/2000 x 2)
7/2400 vs 6/2400 (3/1200 x 2) (clesrovimab trial #1)
8/450 vs 4/450 (clesrovimab trial #2)
27/6850 vs 18/6850 total
Even though I cheated and combined different drugs, and multiplied by 2 which inflated the p value, it still didn’t help - the p value is still 0.18 - still due to chance.
And a reminder - for context, here is the efficacy - clesrovimab reduces the medically attended lower respiratory tract infections (MALRI) by 60%. Some measures like total hospitalizations, even more - 84%.
Fourth question - why was 8 vs 4 not part of MacNeil’s presentation? Perhaps CDC decided to keep this out to avoid unnecessary questions and… rabbit holes from the new ACIP. That backfired. Lesson learned - do not hide things.
And fifth, I have a conspiracy theory of my own. Remember Aaron Siri, the lawyer for Del Bigtree’s ICAN, who was sitting close to Levi in the November 2021 roundtable? Let’s say they kept in touch. On January 25, 2025, Siri’s law firm sent a letter on behalf of ICAN to HHS, that says, “Specifically, we encourage you to closely review the data that showed double
the number of infant deaths among the treatment groups for both Clesrovimab studies.” (my highlight). Note the math error they are making - as we discussed, with 2:1 randomization, 7 vs 3 in the first clesrovimab trial is not an imbalance.
A few weeks after the letter, Levi posted his “concerns” with nirsevimab on x. And at ACIP, he calls 7 vs 3 an “imbalance,” repeating ICAN’s math error. An MIT professor not understanding how to multiply by 2? Or not wanting to disagree with ICAN?
Finally, Levi made a concluding statement. (Remember the Lancet video, 33 million hospitalizations, over 100,000 deaths due to RSV globally - just for context). I encourage you to watch it - starting at 27:57 here:
I’m a scientist, but I’m also a father of six children. And I think it’s also important to put yourself in the shoes of a parent. One of the things that makes me… beyond the science, the data, I was asking myself - if I was just a young parent of a baby, and I had the amazing opportunity to be in this situation 6 times - and I know all the information, how would I think about this dilemma? And I think if I had a baby that was born early, and had God forbid some underlying conditions, knowing the threat that RSV can pose to a baby like that, I would probably use these products to protect my child from this disease since it can cause death to the baby. On the other hand, if I was the father of a healthy child, knowing all of this, I would be concerned to use that. And I think I understand that we are trying to reduce the burden of hospitalizations and these are all very important metrics. But I think we need to ask ourselves, what a parent would say given these data? And I think most parents that have a healthy baby would be concerned to use a new product against the disease that turned out in the past to be quite tricky. I think they will be concerned. And as a father I can feel that I would be concerned.”
First, it’s not clear what he means whey he says “to use that” - is he talking about both antibodies? Or just clesrovimab? Second, the only imbalance that is evident for clesrovimab is 8 to 4 in the trial #2 which is in infants with comorbidities. So if he thinks it’s a real difference (which we know it’s due to chance), the logical thing would be NOT to use it in children with comorbidities, the opposite of what he proposed.
Finally, I was talking to a colleague, an expert in vaccine hesitancy, and I mentioned I will try to interview Levi. “Please remind him that the whole world is watching,” she said. “See if you can explain this to him - he is a mathematician.” “Ah - I know,” I said. “I will tell him, ‘multiply by 8 billion.’”
What I would ask Levi is simple: talk to experts before you make a statement. Ask questions before the televised meeting. Don’t hold your questions (with mix-ups and all) for months. And most importantly, assume positive intent. There is no conspiracy. There are simple explanations for most things. People are not trying to cover things up, just trying to do their job.
I will end by discussing the interview Levi gave, along with Malone, on Epoch TV on Saturday. I heard that Kennedy was “livid” after the ACIP meeting - perhaps too many “Yes” votes? So this interview was perhaps an explanation to the Boss.
For those of you not familiar with Epoch Times, my mom used to love their news site. When I learned this, I asked her to stop. She said, “Why? I like it.” I sent her this:
Further, the Epoch Times frequently publishes pseudoscience news, such as Supernormal Abilities Developed Through Meditation: Dr. Dean Radin Discusses. They also publish false claims from Pseudoscience and anti-vaccination activist Joeseph Mercola who has a long track record of publishing misinformation. Finally, …NBC News report states, “In addition to claims that alien abductions are real and the “deep state engineered the drug epidemic,” the channel pushes the QAnon conspiracy theory, which falsely posits that the same “Spygate” cabal is a front for a global pedophile ring being taken down by Trump.”
Jan Jekielek (pronounced yah-KELLOG) is their Senior Editor and the producer of a 2023 documentary “The Unseen Crisis: Vaccine Stories You Were Never Told.” (On his bio page he shortened it to “The Unseen Crisis.”) The documentary features familiar characters - Senator Ron Johnson and the leaders of the pro-ivermectin group FLCCC (now renamed IMA) - Pierre Kory, Robert Malone, Paul Marik, Peter McCullough, Warner Mendenhall.
I was at a recent IMA conference where I met Jekielek. He moderated a panel. Epoch times was the only media outlet that was allowed at that meeting. I know others tried but were told “no press.” Mendenhall and other lawyers were working the room looking for new clients.
In Saturday’s interview, after a PBS Frontline-style cold open (you can decide which is more credible), and some remarks by Malone, Jekielek turned to Levi. “Retsef, you were very very important for me in terms of my understanding of all sorts of policy around the pandemic.”
This reminds me of my grandmother’s favorite Yiddish saying - az och un vey - which loosely translates as “pity on him.”
“Through speaking with you quite a bit, I understood that I should look at everything from the concept of risk-benefit analysis, whether that’s specific policies, whether that’s products that are being used as interventions because of disease.”
“In my mind the ACIP role is to translate the generic approval by the FDA into a set of more detailed recommendations that take into consideration the risk-benefit aspects that could be different for different subgroups of patients.”
This is not exactly correct. Here is what the ACIP charter says : “The Committee may revise or withdraw their recommendation(s) regarding a particular vaccine as new information on disease epidemiology, vaccine effectiveness or safety, economic considerations, or other data become available.”
To me this is the important part - following disease epidemiology. For example, we don’t have a committee that meets 3 times to review cancer therapeutics. Why? Because cancer epidemiology doesn’t change so quickly. But in infectious disease, changes happen rapidly, epidemics come and go, and the FDA is not able to be involved on such a frequent basis, hence ACIP. But the idea is not for the FDA to approve a new therapy, in a months-long process that involves review of gigabytes of data in hundreds of thousands of pages, literally, and then 2 weeks later an ACIP committee member who has not even read the summary of FDA review says, “Nah, I don’t think so.”
Levi sounds very impressive - “I’ve been in academia from 2006. I have a PhD in Operations Research from Cornell University. This is a discipline that is focused on trying to use data and models that inform complex decisions that involve risk-benefit tradeoffs. It’s using a lot of statistics, a lot of artificial intelligence, a lot of machine learning, a lot of different methodologies…”
As he talks, I cannot help but think about the red “bump” on the graph and no Table 1.
“The main role that I will try to help with is to communicate to patients and medical professionals what is the best knowledge that we have.”
Malone jumped in with more praise: “First, I want to address the issue of the modest Dr. Levi. What he didn’t mention is that he’s bloody brilliant. He is a full professor at the Massachusetts Institute of Technology in data science and data evaluation. That’s no small achievement. Furthermore, he was quite brave and bold throughout the coronavirus crisis. In speaking his truth, he has revealed himself to be an independent thinker and not swayed by proven narratives or conventional thought. I think that the nation is really blessed by having such a mind with these capabilities serving in this way. I don’t know that there has been this level of capability in data analysis before.”
Really?
And the scientific community?
“I’m not sure we have been thinking deeply enough,” Levi said.
Az och un vey.